Peripheral Nerve Injuries
Other Peripheral Nerve Injuries
Peripheral nerves are the structures connecting the spinal cord with different organs, mainly skin and muscles. These nerves run along the extremities.
Injury to these nerves can lead to severe physical and functional disability. These limitations can be totally or partially solved with an adequate treatment performed on time.
CAUSES
There are different causes of injury to these nerves:
- Blunt trauma: blows or trauma without cuts to the skin. There is usually a nerve traction mechanism. For example, in shoulder dislocations, injury to the axillary nerve by this mechanism is common.
- Open trauma: with wounds or cuts in the skin. A sharp object usually cuts the nerve. Sometimes certain surgeries can damage nerves by this mechanism. For example, when placing a hip or knee prosthesis, the femoral nerve or sciatic nerve can be injured.
- Compression: It is produced by ligaments, which in a normal situation, envelop the nerves. The most frequent nerve compression is carpal tunnel syndrome. It is produced by compression of the median nerve in the wrist.
- Inflammation: There are different theories about the possible causes of nerve inflammation. The autoimmune theory (antibodies that react against our own nerve) or viral (virus infection) are the most widely accepted.
SYMPTOMS
Depending on the location and type of peripheral nerve injury, one or more of the following symptoms may occur:
- Weakness or absence of movement of one or more joints.
- Complete or partial loss of sensation. A feeling of ‘numbness‘, ‘padding‘ or even of not feeling the affected areas.
- Neuropathic pain in the affected limb. This pain is usually described as burning, shooting or electric shock-like pain, with different intensity and duration in the affected limb. It responds poorly to regular pain relievers.
EXAMPLES OF PERIPHERAL NERVE INJURIES:
- Axillary nerve: usually injured after dislocations or shoulder surgeries. Its lesion produces weakness of the shoulder.
- Accessory nerve: Usually injured after biopsies or removal of lesions in the neck. Its lesion produces weakness of the shoulder.
- Median nerve: the most typical injury is compression at the wrist. Also known as carpal tunnel syndrome. It produces loss of sensation in the thumb, index finger and middle finger.
- Ulnar Nerve: Typically damaged by compression at the elbow. It produces loss of sensation in the ring and little fingers.
- Radial nerve: usually injured after fractures of the humerus. It produces a “dropped hand,” or deficit to raise (extend) the wrist and fingers.
- Peroneal nerve: usually injured at the knee. It produces the “foot drop”, or deficit of raising the foot.
- Sciatic nerve: It is usually injured after surgery on the thigh.
DIAGNOSIS
The diagnosis of a peripheral nerve injury is based on:
- Clinical history: information told by the patient. For example: a loss of strength for several years can be associated with a tumor or compression in nerve; acute symptoms (sudden in onset) are usually associated with trauma (dislocations, blows, etc.) on the nerves.
- Physical examination: assessment of the strength and sensation of the affected limb.
- Electrophysiological studies: they help determine the type and location of the nerve injury.
- Imaging studies: MRI, ultrasound, or other imaging tests may be necessary to visualize the damaged nerve.
SURGICAL TREATMENT
The following concepts are important to understand:
WHEN TO PERFORM SURGERY
A muscle that is not connected to the nerve atrophies over time. After 1 year the muscle cannot be recovered. On the other hand, if the nerve is in continuity (it is not cut), spontaneous recovery of the nerve and muscle is possible over time without surgery. The nerve grows at a rate of 1 mm / day, starting from the third week after the trauma.
The balance between “waiting” for spontaneous nerve recovery and “not waiting – performing surgery” is complex and must be decided by a peripheral nerve and brachial plexus specialist.
If the nerve is sectioned or if there are doubts about its continuity, surgery should be performed to visualize the nerve as soon as possible. A cut nerve will not regenerate over time. However, if the nerve is in continuity it may be reasonable to wait and see if there is spontaneous regeneration. As a rule, the final decision on whether to perform a surgical intervention should be made in the first 6 months.
It is important to note that surgery of these characteristics, due to its complexity, usually requires careful planning. For this reason, it is important to consult a team specialized in peripheral nerve and brachial plexus as soon as possible.
HOW TO PREPARE FOR SURGERY
- No smoking or other toxic habits: tobacco and other toxic substances have shown delayed nerve recovery.
- Rehabilitation is essential. Systematically perform the exercises recommended by your specialist to avoid joint stiffness. Even though the nerve regenerates and the muscle work again, you will not be able to make movements if the joint is stiff and without mobility.
SURGICAL TECHNIQUES
NEUROLYSIS
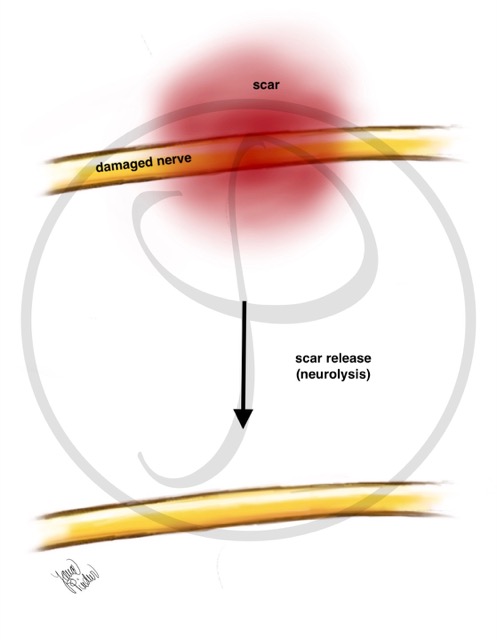
Neurolysis consists of removing all the scar that surrounds the damaged nerve. This is usually required in blunt trauma (for example, after a dislocated elbow without skin injury).
NEUROLYSIS
When a nerve is damaged, a scar appears around it that prevents its proper functioning. Neurolysis is the surgical technique that removes this scar, freeing the nerve to regenerate.
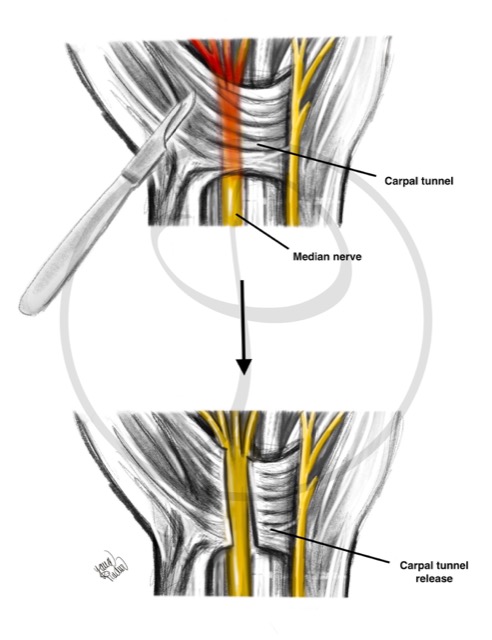
NERVE DECOMPRESSION
Freeing the nerve from an anatomical structure (usually a ligament or tendon).
NERVE DECOMPRESSION
Releasing a nerve that is compressed by a ligament causes its recovery. This occurs in the carpal tunnel syndrome, where the median nerve is “trapped” at the level of the wrist.
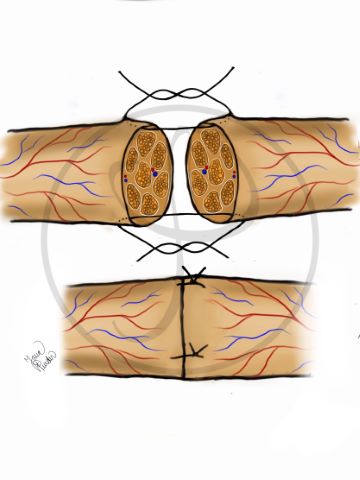
NEURORRHAPHY
Neurorrhaphy consists of joining the ends of the divided nerve. This procedure requires a microscope and a very fine suture (thread) to join the ends of the nerve. It is required in wounds with a cut nerve.
NEURORRHAPHY
Using a very fine thread, the ends of the cut nerve are joined under a microscope.
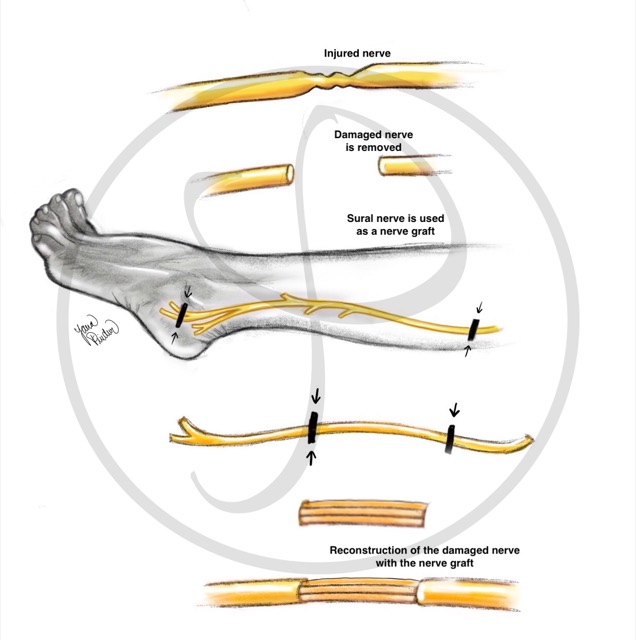
NERVE GRAFT
Obtaining a nerve from another location to repair the gap between the two ends of a cut nerve (as a ‘bridge’). This technique is used when the nerve has been injured and there is a separation between the two ends that does not allow direct coaptation.
The sural nerve is usually the donor nerve. This nerve is responsible for the sensation of the external part of the foot, so its use leaves minor sequelae.
NERVE GRAFT
The sural nerve (leg nerve) can be used to bridge a nerve that has been damaged (from the brachial plexus or from any other location).
NERVE TRANSFER
Nerve transfer consists of joining a part of a healthy nerve to the damaged nerve. This technique is used when the nerve section is too far from the muscle to be reinnervated (reconnected), or in cases where the proximal end of the nerve is not available (typical in high-energy trauma, such as in motorcycle accidents over 100 km/h).
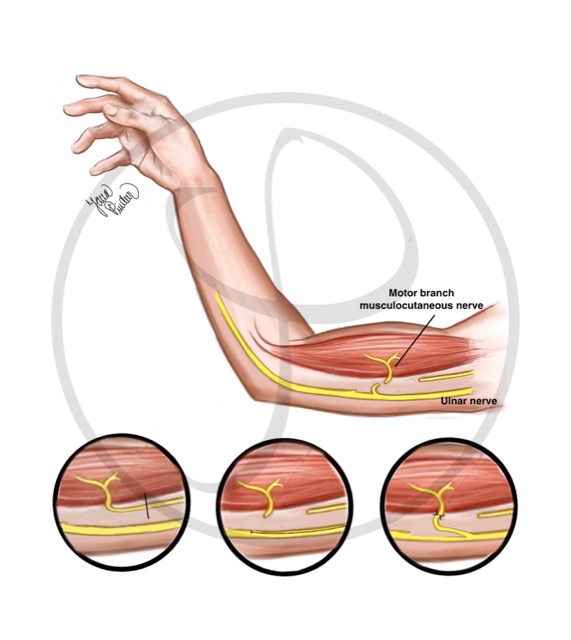
NERVE TRANSFER
It consists of connecting a part of a healthy nerve to a nerve that has been injured. In this figure, a part of the ulnar nerve (nerve without injury) is connected to the musculocutaneous nerve (previously damaged nerve).
TENDON TRANSFERS
A tendon of a muscle that works is connected with another tendon of a muscle that does not work. This technique is used when nerve reconstruction has not been performed and there is muscle atrophy, for example in chronic injuries, more than one year of evolution.
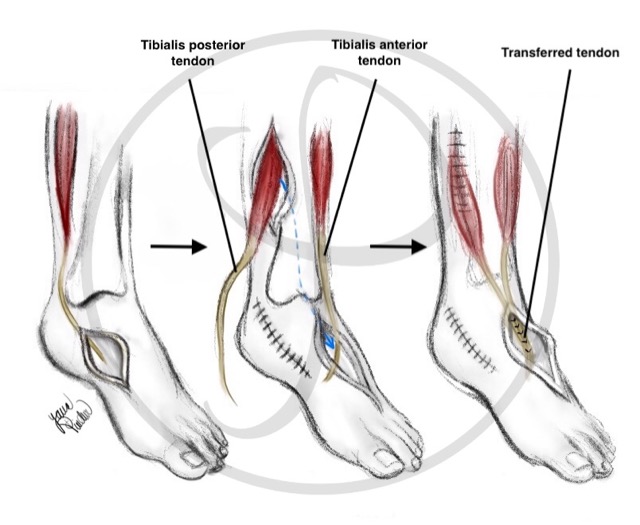
TENDON TRANSFER
It consists of connecting a working tendon to another tendon that has been injured. In this figure, one of the tendons that plantarflexes the foot (posterior tibialis tendon – uninjured tendon) is connected to the tendon that dorsiflexes the foot (anterior tibialis tendon – previously damaged tendon).
FREE MUSCLE TRANSFER
It involves transplanting a muscle from another part of the body to the damaged limb to provide missing function. This technique is used when reinnervation of the damaged muscle is not possible and there is no possibility of a tendon transfer.
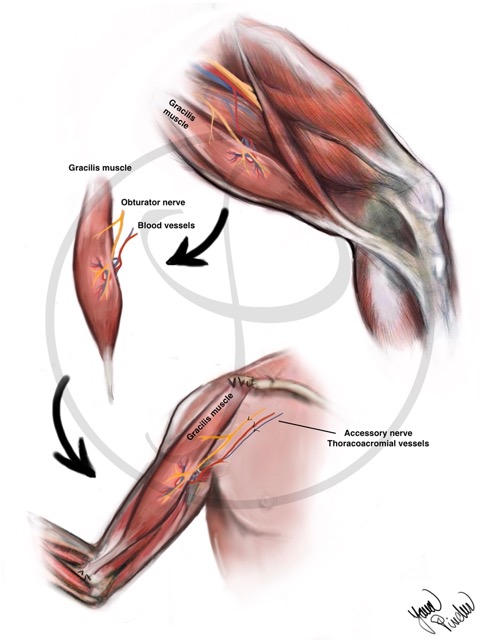
FREE MUSCLE TRANSFER
It consists of transplanting a muscle from another part of the body (generally the leg) to the damaged area. It is necessary to connect the blood vessels of the muscle (they give nutrition) and a nerve
POSTOPERATIVE CARE
After surgery, rehabilitation plays an essential role. Success or failure of the surgery depends on the quantity and quality of the rehabilitation performed. There are 3 phases in the post- surgical period:
- Immobilization phase: a splint is used to immobilize the arm and avoid damage in the repaired nerves. The maximum time is usually 3 weeks.
- Passive mobilization phase: passive exercises to avoid joint stiffness. It begins after the immobilization phase until an active movement of the joint is possible.
- Active mobilization phase: Exercises to activate the target muscle. They should be started after the immobilization phase. Sometimes it takes more than 1 year to get active movement of the affected muscle. Due to the long period of this phase, a high degree of patient motivation is crucial.
WHAT TO DO IF YOU SUSPECT A NERVE INJURY
- Visit a Brachial Plexus and Peripheral Nerve Specialist: although it is not an emergency, you should find a specialist team over the next few days or weeks.
- Rehabilitation is essential. Systematically perform the exercises recommended by your specialist. Even though the nerve regenerates, and the muscle works again, you will not be able to move the affected limb if the joint is stiff and without mobility.
- Live healthy. Do not smoke (tobacco has shown delayed nerve recovery) or take other toxic substances (alcohol). Eat a balanced diet.
- If you experience pain, see a pain specialist. The pain from this type of injury usually improves over time. However, it can be very disabling and complex to treat. Visiting a pain specialist could help to improve your quality of life.