Brachial plexus injuries
Brachial plexus injuries
The upper extremities (arms) and lower extremities (legs) are connected to the spinal cord and brain by a complex system of peripheral nerves.
These nerves send information for movement or sensation. There are five nerve roots (C5-T1 roots) called the brachial plexus. They connect the muscles of the shoulder, elbow, and hand to the spinal cord.
Functional deficits in the limb appear when these nerves are stretched, compressed or, in more severe cases, torn or sectioned.
CAUSES
There are different causes of injury to these nerves:
- High-energy trauma: the most frequent are car or motorcycle accidents. They usually have a worse prognosis than those with lower energy, and usually require reconstructive surgery.
- Low-energy trauma: for example, after shoulder dislocation. They tend to have a better prognosis.
- Inflammatory: There are different theories about the causes of nerve inflammation. The autoimmune theory (antibodies that react against our own nerve) or viral (virus infection) are the most widely accepted.
- Compression: Compression of the brachial plexus nerves is infrequent. It is produced by ligaments or anatomical structures that normally surround the nerves.
TYPES OF INJURIES
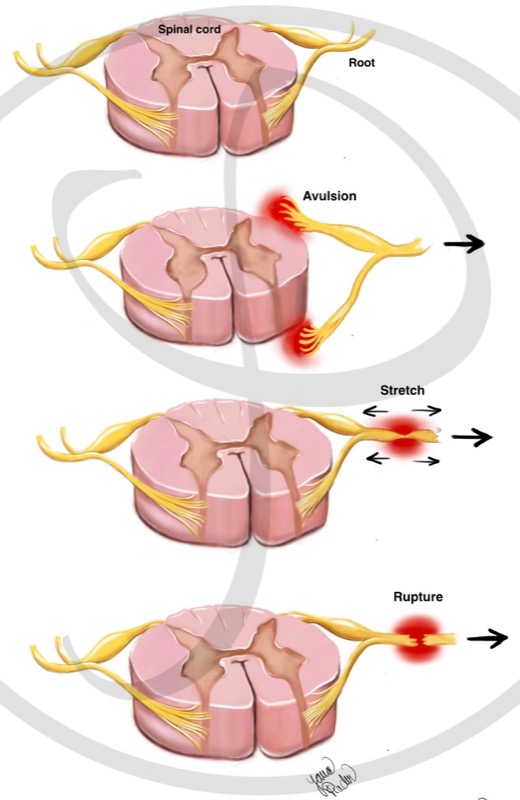
Nerve injury can be caused by different mechanisms. The type of treatment will be determined by causative mechanism. There are 3 types of injuries:
- Nerve avulsion: it is a pulling out of the nerve roots of the medulla.
- Nerve stretch: The nerve is still connected to the spinal cord and is in continuity. However, it cannot transmit information due to injury within the nerve itself.
- Nerve section (rupture): The nerve is connected to the spinal cord, but it is not in continuity (it is cut).
MECHANISMS OF NERVE ROOT INJURY:
There are three types of nerve root injuries. Avulsion is the most severe injury, because it is not possible to connect the nerve to the spinal cord. The stretch and section (rupture) of the nerve are less severe.
SYMPTOMS
Depending on the location and type of peripheral nerve injury, one or more of the following symptoms may occur:
- Weakness or absence of movement of one or more joints.
- Complete or partial loss of sensation. A feeling of ‘numbness‘, ‘padding‘ or even of not feeling the affected areas.
- Neuropathic pain. This pain is usually described as burning, shooting or electric shock like pain, with different intensity and duration in the affected limb. It responds poorly to regular pain relievers.
DIAGNOSIS
The diagnosis is made based on:
- Clinical history: information told by the patient. For example: the speed of the motorcycle during trauma or associated injuries can help determine the degree of
nerve injury. - Physical examination: assessment of the strength and sensation of the affected limb.
- Electrophysiological studies: they help determine the type and location of the nerve injury. They are useful to differentiate avulsion injuries vs. stretching or rupture of the nerve.
- Imaging studies: MRI should be done 3-4 weeks after injury. Level and type of injury (avulsion vs stretching or rupture) can be distinguished.
SURGICAL TREATMENT
Before explaining the possible types of surgery, it is important to understand the following concepts:
WHEN TO PERFORM SURGERY?
A muscle that is not connected to the nerve atrophies over time. After 1 year the muscle cannot be recovered. On the other hand, if the nerve is in continuity (it is not cut), spontaneous recovery of the nerve and muscle is possible over time without surgery. The nerve grows at a rate of 1 mm / day, starting from the third week after the trauma.
The balance between “waiting” for spontaneous nerve recovery and “not waiting – performing surgery” is complex and must be decided by a brachial plexus specialist. As a rule, surgical treatment should be carried out in the first 6 months after the injury.
It is important to note that surgery of these characteristics, due to its complexity, usually requires careful planning. For this reason, it is important to consult a brachial plexus specialist team as soon as possible.
AVAILABLE NERVES FOR RECONSTRUCTION
When planning a reconstruction, it is important to know which nerves are potentially donors. In a nerve avulsion, the damaged root cannot be used since it is not possible to reconnect a nerve root to the spinal cord. Therefore, it is necessary to look for nerves that supply this function. In cases where no nerve of the arm works (complete brachial plexus injuries – they are the most severe), nerves out of the brachial plexus (the spinal nerve or intercostal nerves) can be used.
PRIORITIES IN RECONSTRUCTION
In cases where there is a limitation of available nerves (for example, in complete brachial plexus injury), it is important to prioritize the muscles to be recovered. As a rule, the most important movements are: flexion of the elbow; external rotation or abduction of the shoulder and hand grasp.
SURGICAL TECHNIQUES
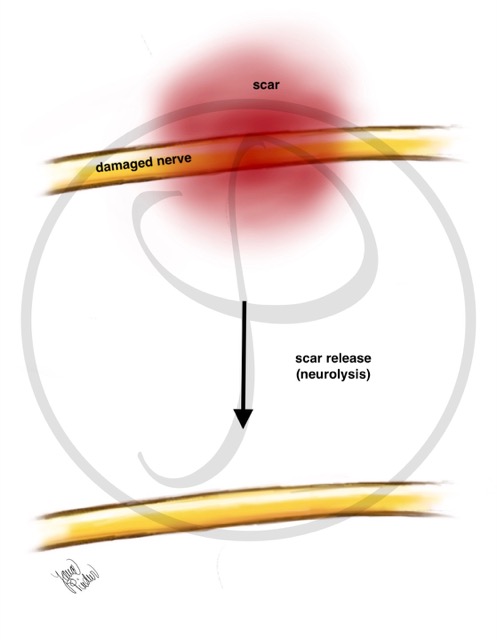
NEUROLYSIS
Neurolysis consists of removing all the scar that surrounds the damaged nerve. This is usually required in blunt trauma (for example, after a dislocated elbow without skin injury).
NEUROLYSIS
When a nerve is damaged, a scar appears around it that prevents its proper functioning. Neurolysis is the surgical technique that removes this scar, freeing the nerve to regenerate.
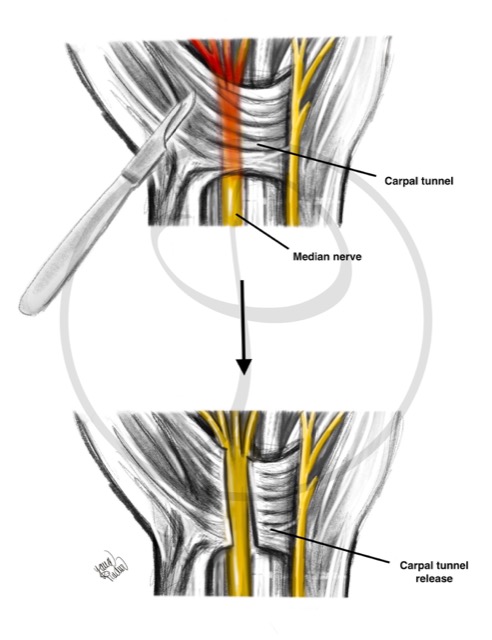
NERVE DECOMPRESSION
Freeing the nerve from an anatomical structure (usually a ligament or tendon).
NERVE DECOMPRESSION
Releasing a nerve that is compressed by a ligament causes its recovery. This occurs in the carpal tunnel syndrome, where the median nerve is “trapped” at the level of the wrist.
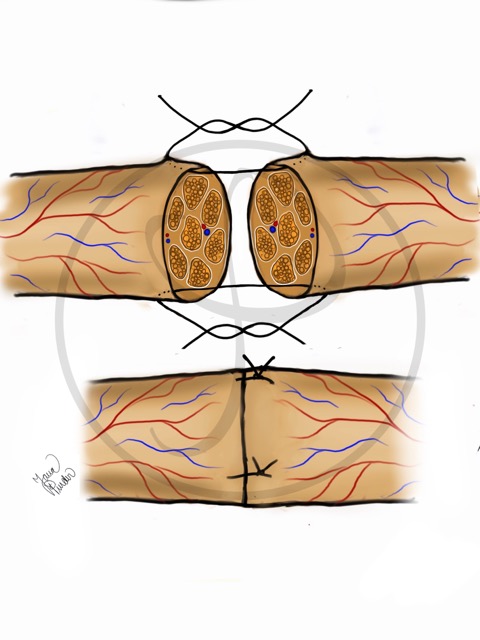
NEURORRHAPHY
Neurorrhaphy consists of joining the ends of the divided nerve. This procedure requires a microscope and a very fine suture to join the ends of the nerve. It is required in wounds with a cut nerve.
NEURORRHAPHY
Using a very fine thread, the ends of the cut nerve are joined under a microscope.
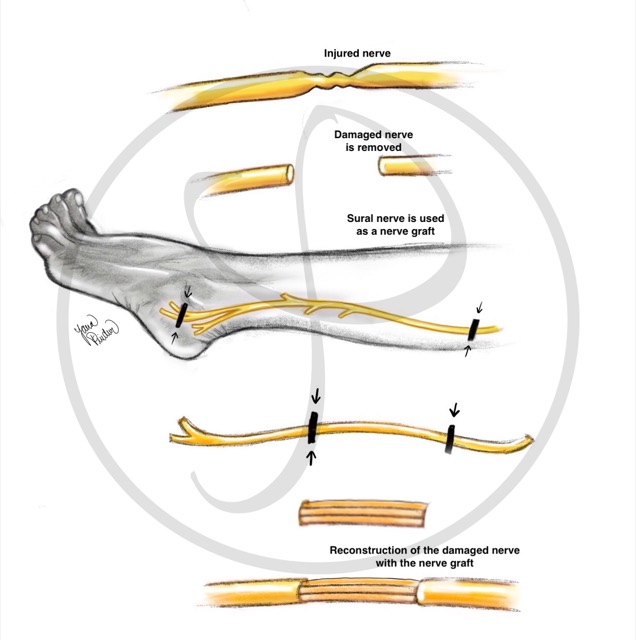
NERVE GRAFT
Obtaining a nerve from another location to repair the gap between the two ends of a cut nerve (as a ‘bridge’). This technique is used when the nerve has been injured and there is a separation between the two ends that does not allow direct coaptation.
The sural nerve is usually the donor nerve. This nerve is responsible for the sensation of the external part of the foot, so its use leaves minor sequelae.
NERVE GRAFT
The sural nerve (leg nerve) can be used to bridge a nerve that has been damaged (from the brachial plexus or from any other location).
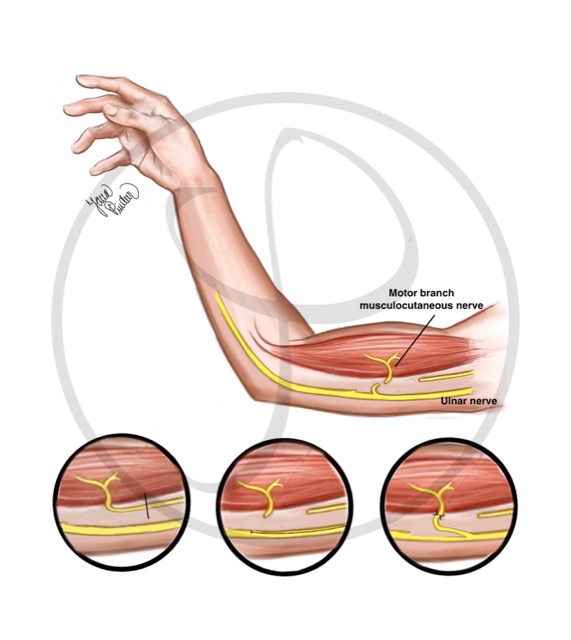
NERVE TRANSFER
Nerve transfer consists of joining a part of a healthy nerve to the damaged nerve. This technique is used when the nerve section is too far from the muscle to be reinnervated (reconnected), or in cases where the proximal end of the nerve is not available (typical in high-energy trauma, such as in motorcycle accidents over 100 km/h).
NERVE TRANSFER
It consists of connecting a part of a healthy nerve to a nerve that has been injured. In this figure, a part of the ulnar nerve (nerve without injury) is connected to the musculocutaneous nerve (previously damaged nerve).
TENDON TRANSFERS
A tendon of a muscle that works is connected with another tendon of a muscle that does not work. This technique is used when nerve reconstruction has not been performed and there is muscle atrophy, for example in chronic injuries, more than one year of evolution.
TENDON TRANSFER
It consists of connecting a working tendon to another tendon that has been injured. In this figure, one of the two tendons that extends (stretches) the index finger (uninjured tendon) is connected to the tendon that moves the thumb (previously damaged tendon). With permission from Maldonado AA, Pindur L, «Treatment of nerve injuries associated with elbow procedures» en «Peripheral nerve issues after Orthopedic Surgery: A multidisciplinary approach to prevention, evaluation and treatment», Springer, 2021
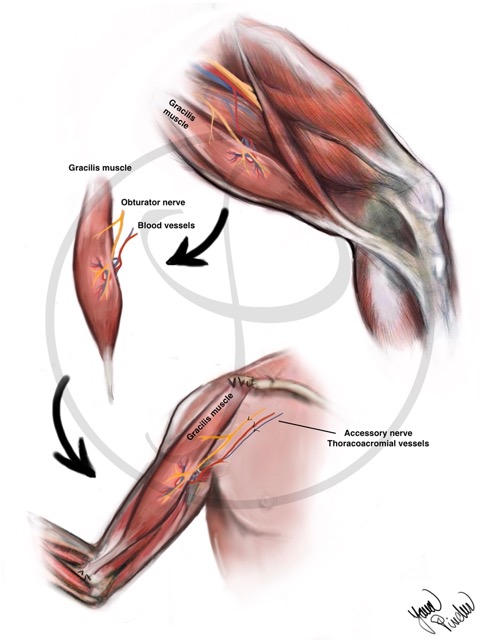
FREE MUSCLE TRANSFER
Involves transplanting a muscle from another part of the body to the damaged limb to provide missing function. This technique is used when reinnervation of the damaged muscle is not possible and there is no possibility of a tendon transfer.
FREE MUSCLE TRANSFER
It consists of transplanting a muscle from another part of the body (generally the leg) to the damaged area. It is necessary to connect the blood vessels of the muscle (they give nutrition) and a nerve.
SECONDARY SURGERIES
To improve the limb function, sometimes it is necessary to perform other interventions after the first surgery. These procedures usually consist of contracture release and tendon transfers (previously described).
POSTOPERATIVE CARE
After surgery, rehabilitation plays an essential role. Success or failure of the surgery largely depends on the quantity and quality of the rehabilitation performed. There are 3 phases in the post-surgical period:
- Immobilization phase: a splint is used to immobilize the arm and avoid damage in the repaired nerves. The maximum time is usually 3 weeks.
- Passive mobilization phase: passive exercises to avoid joint stiffness. It begins after the immobilization phase until an active movement of the joint is possible.
- Active mobilization phase: It consists of activating the affected muscle and nerve. Exercises to try to activate the muscle should be initiated after the immobilization phase. Sometimes it takes more than 1 year to get active movement of the affected muscle. Due to the long period of this phase, a high degree of patient motivation is crucial.
WHAT TO DO IF YOU SUSPECT A BRACHIAL PLEXUS INJURY
1. Visit a Brachial Plexus Injury Specialist – Although it is not an emergency, you should find a specialist team over the next few days or weeks.
2. Rehabilitation is essential. Systematically perform the exercises recommended by your specialist. Even though the nerve regenerates, and the muscle works again, you will not be able to make movements if the joint is stiff and without mobility.
3. Live healthy. Do not smoke (tobacco has shown delayed nerve recovery) or take other toxic substances (alcohol). Eat a balanced diet.
4. If you experience pain, see a pain specialist. The pain from this type of injury usually improves over time. However, it can be very disabling and complex to treat. Visiting a pain specialist could help to improve your quality of life.